Active Surveillance for Early Prostate Cancer
To better understand your symptoms, visit us for a comprehensive diagnosis and personalised treatment plan
Active Surveillance for Early Prostate Cancer
What is prostate cancer?
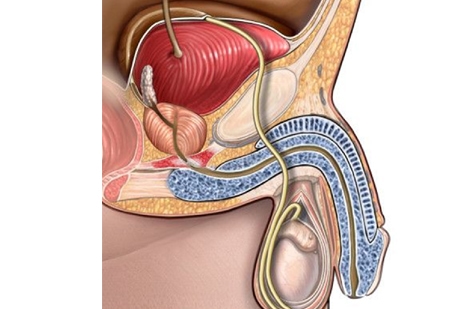
The prostate is a walnut-sized gland that is part of the male reproductive system, and is found below the bladder in the male pelvis (Fig.1). The prostate gland helps produce and store seminal fluid, which is an important component of semen that helps provide nourishment for sperm. Prostate cancer refers to the abnormal uncontrolled growth of cells within the prostate gland, which may then spread outside the prostate to the lymph nodes in the pelvis, and thereafter to the bony skeleton and other parts of the body.
Prostate cancer remains the most common cancer affecting men in the United States, Europe, and Australia. It is the third most common cancer affecting men in Singapore, and is usually diagnosed in men above fifty years of age1. Men with a positive family history of prostate cancer affecting their male relatives are at increased risk of developing prostate cancer themselves.
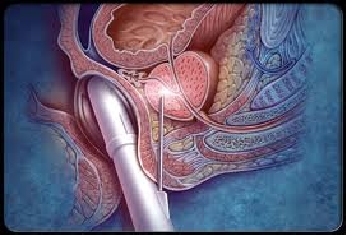
Prostate cancer usually occurs in men aged over fifty years, and becomes more common as men get older. In its early stages, prostate cancer does not cause any symptoms. It is usually detected on finding an abnormally raised serum prostate specific antigen (PSA) level, followed by an ultrasound-guided needle biopsy to confirm or exclude the presence of cancerous cells in the prostate (Fig. 2). With PSA blood tests becoming easily accessible over the last twenty years, the majority of men with prostate cancer are now diagnosed at an early curable stage of their disease. In its advanced stages, prostate cancer may cause obstruction to the urethra with difficulty passing urine; frank blood in the urine (haematuria); blood in the semen (haematospermia); or painful urination. If the cancer has spread to the bony skeleton, patients may experience pain in the back or hips.
Early prostate cancer is an imminently curable disease, and usually carries a very good prognosis if it is detected before the cancer has extended outside the prostate gland. The conventional treatment options are (1) surgery to remove the prostate gland if patients are less than 70 years of age and in good health – in Singapore, this is routinely performed through small incisions using the da Vinci robot (Fig. 3); (2) radiation therapy to ablate the cancer cells in the prostate (Fig. 4); or (3) active surveillance in certain patients whose cancer characteristics have a very low risk of progressing or spreading. For patients choosing curative treatment with surgery or radiation, common side-effects include urinary incontinence (usually a short-lived phenomenon) and impotence.


Active surveillance (AS), as opposed to immediate curative treatment, is a treatment strategy for patients with very early low-risk prostate cancer that aims to reduce unnecessary treatment and its side effects until clinically indicated. Active surveillance protocols aim to achieve the correct timing for curative treatment. This is different from watchful waiting, which was a previous treatment approach of observing prostate cancer patients until they developed symptoms of local or systemic cancer progression. When the latter scenario happened, patients would then be managed palliatively with (1) surgery to unblock prostate or upper tract obstruction; (2) hormonal therapy or (3) palliative radiation for bone metastases. In watchful waiting, prostate cancer patients often miss their window for curative treatment, and in modern clinical practice is usually limited to men of advanced age who are not expected to live more than 10 years.
In active surveillance, patients remain under close follow-up with their urologists, and have their serum PSA levels checked once every 6 months. This is accompanied with an annual prostate biopsy and digital rectal examination to confirm that the prostate cancer cells have not turned more aggressive over the period of surveillance. Should any of these markers show interval progression indicative of aggressive disease, patients are then advised to proceed with curative treatment. In younger men, this means that curative treatment may be delayed for several years until the cancer becomes clinically worrying of aggressive spread.
Most international guidelines recommend active surveillance as a treatment option for patients with clinically confined prostate cancer that has very low risk of cancer progression2,3. The strict criteria for such patients include:
- Life expectancy of more than 10 years
- Clinical stage T1/T2 cancers (ie. prostates with no or very small palpable nodules)
- Serum PSA < 10ng/dl
- Gleason prostate biopsy score of ≤ 6 (out of 10)
- ≤ 2 positive cores on biopsy (minimum of 12 cores taken)
- ≤ 50% cancer involvement per biopsy core
In addition, a consensus meeting recently suggested excluding men from active surveillance if their prostate biopsy reports contained any of the following worrisome characteristics: (1) predominant ductal carcinoma; (2) sarcomatoid carcinoma; (3) extraprostatic extension of cancer; and (4) lymphovascular invasion3 (Fig. 5).

In a recent systematic review of over 3,900 patients, active surveillance was found to be generally safe for the majority of patients with low-risk cancer characteristics as described above5. One of the largest cohorts of AS patients with the longest follow-up reported a 2.8% incidence of developing bony metastases during follow-up. 27% of the cohort eventually underwent curative treatment (either surgery of radiation), when they developed worrying characteristics on follow-up PSA testing and repeat prostate biopsies.
Patients usually drop out of active surveillance programmes and pursue definitive treatment with surgery or radiation for one or more of these 3 reasons: (1) they were found to have worrisome characteristics on follow-up, (2) they found the regular PSA blood tests and repeated prostate biopsies inconvenient or unbearable; or (3) they became anxious that they might miss their “opportunity for cure”. In the latter scenario, such patients find living with the knowledge of having prostate cancer a great psychological burden. For such patients, the prospect of having the prostate surgically removed or radiated seemed inevitable, and they prefer to opt for definitive treatment whilst they are younger and able to recover more quickly, and thereafter to move on with their lives.
PSA screening in healthy populations remains one of the most controversial topics in public health debate. The 2013 Cochrane review summarized the findings of published data from 5 randomized controlled trials as follows7:
- • PSA screening is associated with an increased diagnosis of early stage prostate cancer
- • There is no benefit in either cancer-specific or overall survival in cohorts undergoing PSA screening
- • PSA screening is associated with risk of over-diagnosis and overtreatment
As a result, many countries no longer advocate PSA screening in healthy populations. However, most urologists would still advise patients above the age of 50 years, or those with a positive family history of prostate cancer in their male relatives, to go for annual serum PSA checks.
With technological advances in treatment modalities of prostate cancer leading to much fewer side-effects, the outlook for prostate cancer patients in most cases is very good. With active surveillance now becoming an established safe treatment approach for early very low-risk prostate cancers, many men who are diagnosed early in the course of their disease can be safely monitored for years before the need for curative intervention arises. Unnecessary side effects of overtreatment may thus be avoided until definitive treatment is truly needed.
As such, men above the age of fifty years should not be afraid of having their PSA checked, as earlier diagnosis at an curable stage in most instances carries a much better prognosis, than if men were to wait till they develop symptoms of advanced disease before seeking help.
1. Singapore Cancer Registry Interim Report Trends In Cancer Incidence In Singapore 2008-2012. National Registry of Diseases Office (NRDO).
2. Mottet N, Bellmunt J, Briers E et al. EAU 2015 Guidelines on prostate cancer. European Association of Urology. http://uroweb.org/wp-content/uploads/09-Prostate-Cancer_LR.pdf
3. Ip S, Dahabreh IJ, Chung M et al. An evidence review of active surveillance in men with localized prostate cancer. Evidence Reports Technology Assessments 2011;204: 1 -341.
4. Montironi R, Hammond EH, Lin DW et al. Consensus statement with recommendations on active surveillance inclusion criteria and definition of progression in men with localized prostate cancer: the critical role of the pathologist. Virchow Arch 2014; 465(6): 623-628.
5. Thomsen FB, Brasso K, Klotz LH et al. Active surveillance for clinically localized prostate cancer – a systematic review. Journal of Surgical Oncology 2014; 109(8): 830-835.
6. Klotz L, Zhang L, Lam A et al. Clinical results of long-term follow-up of a large, active surveillance cohort with localized prostate cancer. Journal of Clinical Oncology 2010; 28(1): 126-131.
7. Ilic D, Neuberger MM, Djulbegovic M et al. Screening for prostate cancer. Cochrane Database Systematic Review 2013; Jan 1: CD004720.
