My PSA Is High! What Happens Next, Doc?
To better understand your symptoms, visit us for a comprehensive diagnosis and personalised treatment plan
My PSA Is High! What Happens Next, Doc?
What is the PSA blood test all about? When should I be worried?
The prostate-specific antigen (PSA) blood test for men is a quick way to assess the likelihood of having prostate cancer. Prostate cancer remains the most common cancer affecting men in the United States, Europe, and Australia, and it is the third most common cancer affecting men in Singapore1.
PSA is a protein produced by cells in the prostate gland, and most urologists around the world consider PSA levels of less than 4.0ng/dl as normal. PSA levels higher than 4.0ng/dl are associated with a higher risk of having prostate cancer, although this may also be due to other causes such as prostate enlargement, inflammation of the prostate (prostatitis), recent ejaculation and / or prostate surgery2. The PSA blood test is often done as part of health screening packages for men older than 50 years of age, as the likelihood of prostate cancer increases with age.
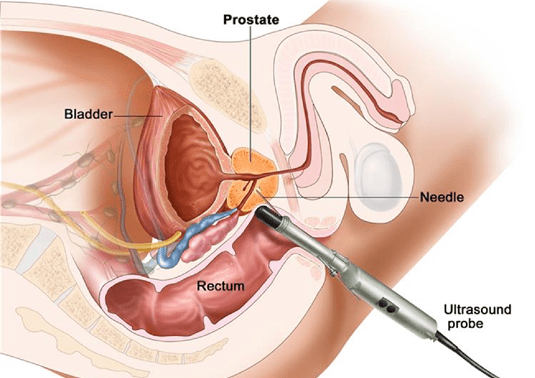
When men are found to have a PSA blood test > 4.0ng.dl, they will often be referred to a urologist for further assessment. The urologist will usually ask about symptoms caused by prostate disease such as slow urinary flow, painful or frequent urination, or visible blood in the urine. He will usually use a bedside ultrasound to measure the size of the prostate gland, followed by a digital rectal examination to feel for possible nodules or areas of inflammation in the prostate. He will then discuss the option of proceeding with a prostate biopsy to obtain cells for histological diagnosis to rule out prostate cancer.
Men whose PSA results fall in the 4.0 – 10.0ng/dl range have a one in seven chance of being diagnosed with prostate cancer on prostate biopsy. However, men whose PSA levels are > 10.1ng/dl have a greater than 50% chance of having prostate cancer, which is oftentimes an aggressive form. For the latter group, they should not delay proceeding with a prostate biopsy to confirm or exclude the presence of cancer cells in the prostate.

In patients with a mildly raised serum PSA of 4.0 – 10.0ng/dl, the likelihood of finding clinically significant prostate cancer is less than 15%. In this group of patients, their urologist may suggest a trial of antibiotics and medications for suspected prostatitis first, before repeating their PSA test 6-8 weeks later to see if it has fallen back to normal levels. However, this strategy is not advised for men whose PSA levels are > 10.1ng/dl, as the chance of detecting aggressive prostate cancer is quite high. In the latter group, they should not delay having a prostate biopsy to obtain early histological diagnosis for treatment planning.
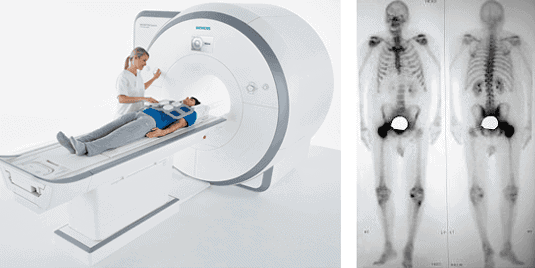 Fig 4. Staging of prostate cancer is usually assessed with (A) Magnetic resonance imaging of the prostate gland and (B) Bone scan.
Fig 4. Staging of prostate cancer is usually assessed with (A) Magnetic resonance imaging of the prostate gland and (B) Bone scan.PSA screening was controversial a few years ago because it identified many men with early indolent prostate cancer, which carries a low risk of spreading outside the prostate gland4. Such men may have been advised to go for treatment such as surgery or radiation, with their consequent side effects.
In 2015, we now have good practice guidelines and clinical data to show that men diagnosed with indolent (low-risk) prostate cancer may be safely monitored in an active surveillance programme (often for many years), until their repeat PSA levels or prostate biopsy reports show aggressive cancerous change. Active surveillance seeks to delay definitive treatment for early prostate cancer till it is clinically necessary, and has been validated in many large long-term studies to be a safe treatment approach5. As such, the Singapore Urological Association continues to encourage men above the age of fifty years to go for their annual PSA blood test. Early detection, surveillance and cure for organ-confined prostate cancer is still a better option than a late diagnosis of advanced prostate cancer, with its bleak outlook and limited treatment options.
1. Singapore Cancer Registry Interim Report Trends In Cancer Incidence In Singapore 2008-2012. National Registry of Diseases Office (NRDO).
2. Mottet N, Bellmunt J, Briers E et al. EAU 2015 Guidelines on prostate cancer. European Association of Urology. http://uroweb.org/wp-content/uploads/09-Prostate-Cancer_LR.pdf
3. National Cancer Institute. Prostate-Specific Antigen (PSA) Test. http://www.cancer.gov/cancertopics/types/prostate/psa-fact-sheet
4. Ilic D, Neuberger MM, Djulbegovic M et al. Screening for prostate cancer. Cochrane Database Systematic Review 2013; Jan 1: CD004720.
5. Thomsen FB, Brasso K, Klotz LH et al. Active surveillance for clinically localized prostate cancer – a systematic review. Journal of Surgical Oncology 2014; 109(8): 830-835.
